Introduction
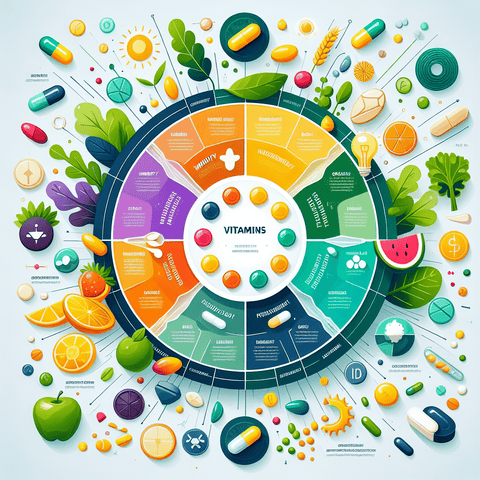
Multivitamins have become a staple in many households, touted as a convenient way to fill in nutritional gaps and maintain overall health. With colorful labels promising energy, immunity, and vitality, it’s not surprising that millions of people reach for them every day. Marketed across age groups, dietary preferences, and lifestyles, multivitamin supplements are among the most widely consumed products in the global dietary supplement market.
However, not everyone benefits from taking multivitamins. In fact, for some individuals, these supplements may do more harm than good. Whether it's due to potential interactions with medications, underlying health conditions, or specific nutrient sensitivities, multivitamins are not a one-size-fits-all solution.
In this article, we will delve into who should not take a multivitamin, the potential risks associated with inappropriate supplementation, and how to make safe, personalized decisions about your vitamin intake. Armed with expert insights and scientific backing, you’ll learn how to navigate the complex landscape of multivitamins with confidence—and caution where needed.
Multivitamin Precautions: What You Need to Know Before Supplementing
Before incorporating a multivitamin into your daily regimen, it’s critical to understand the fundamentals of supplement safety. First and foremost is the importance of dosage. Multivitamins often contain a wide range of vitamins and minerals, but that doesn’t mean that more is always better. Consuming excessive amounts of certain nutrients—even those considered essential—can cause adverse reactions and, in some cases, long-term health complications.
Unfortunately, many over-the-counter multivitamins lack transparency when it comes to ingredient sourcing, manufacturing practices, or potency. Some may contain unnecessary additives or fillers, and in certain cases, may be poorly formulated—offering nutrients in forms that are not well absorbed by the body.
One of the most common misconceptions is that multivitamins are universally harmless. This belief may lead individuals to take them without proper medical advice or consideration of individual needs. If you're already on prescription medication, you must be cautious. For example, certain vitamins can interfere with blood pressure medications, diuretics, or anticoagulants. Adjusting dosage or avoiding supplementation altogether may be recommended depending on your condition and treatment.
Moreover, people with health conditions such as liver or kidney disease must be especially vigilant. Filters like the liver and kidneys are responsible for metabolizing and excreting excess nutrients. Over-supplementation can burden these organs, potentially leading to toxicity or organ stress.
Red flags that may indicate you should stop or reconsider a multivitamin include gastrointestinal discomfort, headaches, skin rashes, or unusual changes in urine color or frequency. These symptoms could signal nutrient imbalances or sensitivities. If any such occurrences arise after starting a supplement, it’s advisable to consult a healthcare provider for guidance and possibly undergo nutritional testing.
Rather than self-diagnosing nutrient deficiencies, it is safer and more effective to assess your dietary intake through food frequency questionnaires or nutrient tracking applications. Blood tests and professional evaluations provide the most accurate picture.
Ultimately, multivitamin supplementation should not be treated as a substitute for a balanced diet rich in whole foods. Instead, it should be considered a targeted tool, best used in cooperation with a knowledgeable healthcare provider, particularly when existing medical conditions or medications are involved.
Potential Adverse Effects of Multivitamins in Certain Populations
Although generally marketed as beneficial, multivitamins can cause a range of adverse effects in sensitive or high-risk populations. These effects may vary in severity depending on an individual’s age, metabolism, overall health, and the specific formulation of the supplement.
Gastrointestinal issues such as nausea, constipation, bloating, or diarrhea are commonly reported during initial multivitamin use. These symptoms are often the result of high doses of iron or magnesium. Magnesium, although an essential mineral supporting bone and muscle function, can cause digestive disruption when taken in large amounts without food.
Allergic reactions are another concern, particularly when supplements include added colors, fillers, or herbal extracts. Sensitive individuals may experience itching, hives, or even anaphylaxis. Ingredients like soy, dairy, gluten, and shellfish are not always declared clearly on labels but may be present as trace contaminants or base ingredients.
Certain populations may experience more significant risks. For example, smokers or people exposed to asbestos have been shown to experience increased cancer risks when consuming high-dose beta-carotene supplements. Similarly, excessive vitamin A intake can lead to hypervitaminosis A, characterized by dry skin, bone pain, dizziness, and liver abnormalities. Such risks underscore the importance of understanding both the dosage and form of nutrients included in any multivitamin.
Long-term health implications are perhaps the most concerning. An overload of fat-soluble vitamins—namely vitamins A, D, E, and K—can lead to nutrient build-up in body tissues, potentially resulting in organ dysfunction. Constant exposure to excessive intake can strain metabolic functions and alter hormonal balances, sometimes irreversibly.
Furthermore, there is growing evidence that multivitamins may interact negatively with pre-existing health conditions. In individuals with thyroid disorders, for instance, iodine or selenium present in multivitamins can exacerbate symptoms or interfere with thyroid medications. Likewise, those with cardiovascular issues must monitor vitamin K intake due to its critical role in blood clotting—a topic we'll discuss further below.
Clearly, multivitamin use is not free from risks. Identifying your individual requirements, considering current health status, and leveraging expert advice can allow for a safer and more effective approach to nutritional supplementation. If adverse effects emerge, discontinuing use and reconsidering nutritional strategies is often the wisest course.
Vitamin Overdose Risks and When They Occur
Not all vitamins are excreted equally. Fat-soluble vitamins—namely vitamins A, D, E, and K—are stored in the body’s fatty tissues and liver. This means that regular consumption above the tolerable upper intake level (UL) can lead to accumulation and eventual toxicity.
Vitamin A toxicity, or hypervitaminosis A, is one of the more well-known overdose conditions. Early symptoms include nausea, headache, fatigue, and blurred vision. Over time, it can lead to bone demineralization, liver damage, and even intracranial pressure. Pregnant women who take excess vitamin A put their unborn child at risk for birth defects, creating further concern about indiscriminate supplement use.
Vitamin D toxicity is another significant public health issue, especially considering the growing popularity of high-dose vitamin D supplements for bone, immunity, and mood. While moderate doses may benefit individuals with proven deficiencies, high levels can disrupt calcium metabolism, resulting in hypercalcemia. Symptoms include kidney stones, confusion, nausea, and even cardiovascular complications. For those seeking support for calcium metabolism or skeletal health, safer alternatives, like moderate-dose vitamin D formulations, should be preferred based on professional recommendations.
Though water-soluble vitamins like the B-complex and vitamin C are generally flushed out of the body when consumed in excess, mega-doses can still cause complications. High levels of vitamin B6 (pyridoxine), for example, have been associated with nerve damage or sensory neuropathy. Vitamin C in excess can trigger gastrointestinal discomfort and has been linked to kidney stone formation in susceptible individuals.
What compounds the risk of overdose is unintentional stacking. Many people take multivitamins alongside fortified foods (such as cereals and juices) or additional single-nutrient supplements. Over time, this layering effect can cause cumulative exposure beyond safe thresholds, even when each product individually appears moderate.
Understanding the signs of vitamin toxicity is essential. Symptoms may include fatigue, joint pain, muscle weakness, irregular heartbeat, and skin discoloration. Given their subtle and nonspecific nature, these symptoms often go unrecognized, further highlighting the need for caution and education.
If you suspect a vitamin overdose, it's crucial to seek medical advice immediately. Blood tests can reveal nutrient imbalances and help recalibrate your supplement usage. Overall, respecting recommended dietary allowances (RDAs) and consulting professionals is the best defense against overdose hazards.
Contraindications for Taking Multivitamins
Several clinical scenarios warrant careful scrutiny before recommending multivitamin use. Some health conditions may be worsened by particular vitamins and minerals, making conflict-free supplementation a tricky balancing act.
Kidney disease is a prime example. The kidneys play a vital role in filtering waste products and excess nutrients. For individuals with impaired renal function, standard multivitamin doses—especially those containing potassium, magnesium, and phosphorus—can contribute to dangerous imbalances or toxicities. Some formulations with preformed vitamin A or high-dose vitamin D can accumulate in such individuals, exacerbating metabolic complications.
Similarly, people with liver disease, such as cirrhosis or hepatitis, must also be careful. The liver is the main detoxifying organ and helps metabolize fat-soluble vitamins. With diminished capacity, the liver struggles to process excess nutrients, increasing the risk of toxicity-related damage. In these cases, professionally supervised supplementation, if any, must be tailored to the individual’s organ capacity and biochemical markers.
Certain metabolic disorders—like hemochromatosis, which causes excess iron absorption—render iron-rich multivitamins unsafe. In this case, iron supplementation can lead to oxidative stress, joint damage, and liver complications.
Furthermore, multivitamins may interact negatively with ongoing medical treatments. Blood-thinning drugs like warfarin can become less effective when combined with high doses of vitamin K, which plays a pivotal role in clot formation. Calcium and magnesium can bind to antibiotics such as tetracycline or ciprofloxacin, reducing their efficacy. Even anti-retroviral treatment and chemotherapy protocols often come with specific nutrient-related contraindications.
Food and environmental allergies add yet another layer of complexity. Hidden allergens in multivitamin capsules might trigger unwanted immune responses—essentially turning a health-promoting product into a hazardous one. Look for allergen-free products that are tested for purity with clear ingredient disclosures. Consultation with an allergist or immunologist may be necessary in high-risk individuals.
Special populations, including pregnant women or post-operative patients, require expert supervision. Nutrient demands and tolerances in such situations are unique, and wrong dosages can lead to nutrient imbalances or toxicity. Medical oversight ensures micronutrient delivery is both safe and therapeutic.
The bottom line? Not all bodies function the same way, and underlying conditions alter how nutrients are processed. When contraindications exist, it's critical to pursue a customized supplementation plan—ideally under professional medical care—to ensure no harm is done.
Nutrient Interactions and Their Impact on Efficacy and Safety
While multivitamins are designed to offer a comprehensive nutrient profile, the interaction between certain ingredients can influence their absorption, effectiveness, and safety. Without proper formatting or balance, these interactions can lead to subpar results—or worse, unintended side effects.
One of the most well-known nutrient conflicts is between calcium and iron. These two minerals compete for the same absorption pathways in the gut. When taken together, calcium can significantly reduce the bioavailability of iron, rendering it less effective. This interplay is particularly concerning for individuals at risk of anemia or poor bone health.
Vitamin K poses another vital consideration, particularly regarding pharmaceuticals. It is known to interfere with anticoagulant therapy, altering clotting times and raising the risk of either bleeding or clotting complications. People on blood thinners are advised to maintain stable, consistent levels of vitamin K, avoiding large fluctuations commonly introduced by multivitamins.
Magnesium, while essential for muscle and nerve function, can form insoluble compounds with some antibiotics and osteoporosis medications. This inhibits drug absorption and renders treatment less effective. A well-formulated magnesium supplement like those found here should include user guidelines and interactions for optimal timing and dosing.
Another set of interactions arises between zinc and copper. Excessive zinc intake can impair copper absorption, leading to deficiency symptoms over time. Likewise, vitamin C can enhance non-heme iron absorption but may exacerbate iron overload conditions, such as hemochromatosis.
Understanding these nutrient dynamics reinforces the importance of not indiscriminately combining multiple supplements or fortified foods. More is not always better, and in some cases, the presence of one vitamin can defeat the purpose of another. Balanced formulations crafted with precise ratios help ensure nutrient synergy instead of interference.
Consumers are encouraged to read labels, cross-reference with their current regime, and if necessary, work with a qualified nutritionist or pharmacist. Only then can supplements fulfill their intended role of supporting rather than compromising your health.
Special Populations and Their Unique Safety Considerations
Different life stages and physiological conditions demand different nutritional profiles—and risk factors. Multivitamins must be specifically adjusted for special populations to avoid adverse consequences.
For pregnant and breastfeeding women, nutrient requirements shift dramatically. While folic acid, iron, and iodine are indispensable during pregnancy, excessive vitamin A is strictly contraindicated due to its teratogenic effects. Prenatal vitamins must be carefully formulated, and professional monitoring is essential to avoid defects and complications. Special pregnancy-safe formulations are widely available and should be preferred over standard multivitamins.
Children and adolescents are another group with unique needs and limitations. Their bodies are still growing, and overdoses can disrupt natural development. Chewable or gummy multivitamins must be stored out of reach, as their enticing flavors can tempt accidental overconsumption. Age-appropriate formulations with child-safe dosages and delivery formats are essential.
Elderly adults face a different challenge. Absorption efficiency decreases with age, and medication use increases—creating a complex web of nutrient-drug interactions. Elder adults are particularly vulnerable to vitamin D and B12 deficiencies but must still moderate intake of fat-soluble vitamins to avoid metabolic dysfunction. Professionally guided supplementation is often integral to aging care plans.
Individuals with chronic illnesses like diabetes, autoimmune disorders, or gastrointestinal conditions require targeted nutrition due to altered metabolic demands and possible digestive impairments. A one-size-fits-all multivitamin may prove insufficient—or dangerous—for these groups.
Athletes and those with physically active lifestyles need tailored nutritional support based on performance output. Higher sweat loss may increase need for electrolytes, while recovery phases may demand specific amino acids or antioxidant support like vitamin C. However, assuming all athletes should consume high-dose multivitamins can be a mistake. Over-supplementation can impair natural adaptation and recovery processes.
Conclusively, every special population has suitable, evidence-based solutions. The safest course of action remains professional consultation and product personalization for optimal safety and effectiveness.
Conclusion
While multivitamins offer a convenient way to enhance nutrition, they are not universally safe or beneficial. Individuals with specific health conditions, those taking certain medications, and diverse population groups like pregnant women, children, and the elderly must approach supplementation with care and deliberation. Recognizing nutrient interactions, potential overdose risks, and contraindications is vital to avoid unforeseen harm.
Your best tool for making informed decisions is knowledge—coupled with the guidance of healthcare professionals who understand your unique biology. Evaluate needs and risks realistically, read labels diligently, and avoid self-medicating with overly broad solutions. Where supplementation is justified, consider targeted, verified, and dosage-aware products from credible sources like TopVitamine’s range of omega-3 fatty acids, vitamin D options, and magnesium supplements.
Personalization isn’t just a modern health trend—it’s a necessity for safe, effective supplement use. The best defense is a proactive, informed mindset.
Q&A Section
Q: Can anyone take a multivitamin without risk?
A: No, certain individuals—including those with kidney or liver disease, pregnancy, or on specific medications—should consult with a healthcare provider before taking a multivitamin to avoid potential complications and nutrient interactions.
Q: What are signs of a vitamin overdose?
A: Symptoms vary depending on the vitamin, but common signs include nausea, fatigue, headaches, blurred vision, digestive upset, and skin issues. Vitamin A and D overdoses are especially dangerous over time.
Q: Are there safe multivitamin alternatives?
A: Yes, targeted or condition-specific supplements like omega-3 fatty acids, vitamin C, or vitamin D can offer more precise benefits without the complex nutrient load of multivitamins.
Q: Should children take multivitamins?
A: Only if recommended by a pediatrician. Children have different nutritional needs and can easily overdose on fat-soluble vitamins through chewables or gummies.
Q: Is it safe to combine multivitamins with other supplements?
A: Combining supplements can lead to unintentional overdoses or nutrient interactions. Always cross-check ingredients and consult a healthcare provider for a harmonized supplement plan.
Important Keywords
- multivitamin safety
- who should not take multivitamins
- vitamin overdose symptoms
- vitamin interactions
- special populations supplements
- contraindications for multivitamins
- multivitamin adverse effects
- fat-soluble vitamin toxicity
- nutrient absorption interactions
- Topvitamine supplements